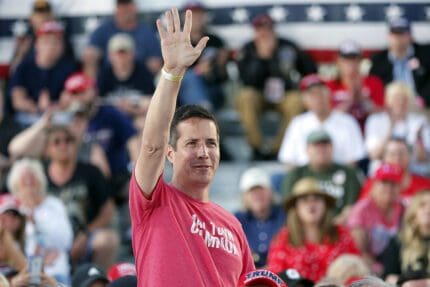
Dr. Rick Bright: Trump administration gave hospitals masks that don't work
Bright told Congress that doctors and nurses got substandard foreign N95 medical masks.

Dr. Rick Bright, the former director of the Biomedical Advanced Research and Development Authority, told Congress on Thursday that the federal government obtained substandard foreign masks that do not keep medical workers safe from COVID-19.
Bright was asked by Rep. Kathy Castor (D-FL) at a House Committee on Energy and Commerce’s health subcommittee hearing about the consequences of the Trump administration’s monthslong delay in mounting an aggressive response to the pandemic. Bright answered that, “lives were endangered, and I believe lives were lost.”
“Not only that, they were forced to procure the supplies from other countries, without the right quality standards,” Bright said. “So even our doctors and nurses in the hospitals today are wearing N95-marked masks from other countries, that are not providing the sufficient protection that a U.S. standard N95 mask would provide them. Some of those masks are only 30% effective. Nurses are rushing in the hospitals thinking they’re protected — and they’re not.”
Bright was testifying as a whistleblower at Thursday’s subcommittee hearing on “Protecting Scientific Integrity in the COVID-19 Response.”
The former head of vaccine development for within the Health and Human Services Department, he was demoted by the Trump administration after urging more stringent testing of hydroxychloroquine before recommending it as a treatment for COVID-19 and opposing a plan to flood New York and New Jersey with the drug. Trump repeatedly touted the anti-malarial medication as a “miracle” cure for the coronavirus, though studies have not shown it to be an effective treatment.
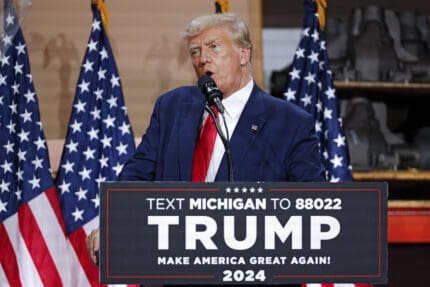
On Thursday, Trump attacked Bright as a “disgruntled employee” who is “not liked or respected by people I spoke to.”
The N95 face masks Bright mentioned are personal protective equipment, also known as PPE, designed to protect medical workers by filtering out germs and other particles. Throughout the pandemic, a shortage of these masks has left medical providers insufficiently protected as they attempt to treat the 1.3 million-plus people with COVID-19 and others.
Unable to get sufficient PPE, hospitals sought to acquire masks from outside their typical supply chain. Many proved to be supplies substandard.
“These aren’t perfect but they have some protection,” one hospital administrator told the Wall Street Journal in April. “Everything about it looks legit. But the product itself is clearly not.”
Thousands of health care workers have already tested positive for the coronavirus.
Last week, the FDA banned the sale of defective N95-style face masks from more than 65 of the 80 manufacturers in China that had been authorized by the agency.
Published with permission of The American Independent Foundation.
Recommended

Biden campaign launches new ad focused on Affordable Care Act
Former President Trump has said he wants to do away with the popular health care law.
By Kim Lyons, Pennsylvania Capital-Star - May 08, 2024
Ohio doctors fear effects of emergency abortion care case set to go before U.S. Supreme Court
A federal law that allows emergency departments to treat patients without regard to their ability to pay will be under U.S. Supreme Court scrutiny this week, and Ohio doctors are concerned about the case’s local impact on emergency abortion care.
By Susan Tebben, Ohio Capital Journal - April 23, 2024
House GOP votes to end flu, whooping cough vaccine rules for foster and adoptive families
A bill to eliminate flu and whooping cough vaccine requirements for adoptive and foster families caring for babies and medically fragile kids is heading to the governor’s desk.
By Anita Wadhwani, Tennessee Lookout - March 26, 2024